Cannabis users were 3.5 times more likely to have a fungal infection than nonusers, according to an analysis of more than 20 million insurance claims published in Emerging Infectious Diseases. Although researchers were unable to establish causality between cannabis use and fungal infections, they said that their study adds to a growing body of evidence showing a link between the two.
“The frequency of fungal infections associated with cannabis is unknown but is a growing concern as more states legalize its medicinal and recreational use,” Kaitlin Benedict, MPH, an epidemiologist in the Mycotic Diseases Branch of the CDC, and colleagues wrote.
The researchers analyzed claims data to determine the prevalence of the mold infections aspergillosis and mucormycosis among cannabis users and nonusers. They also looked for the fungal infections blastomycosis, coccidioidomycosis, cryptococcosis and histoplasmosis in both groups. Benedict and colleagues compared clinical and demographic features between users and nonusers. Patients with presumed ocular histoplasmosis syndrome were not included in the analysis.
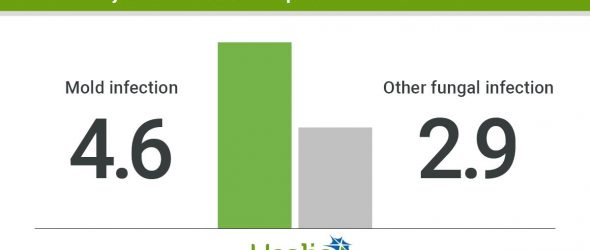
Benedict and colleagues found that in 2016, 40 of 53,217 cannabis users and 6,294 of 21.5 million nonusers had one of the fungal infections (OR = 2.6; 95% CI, 1.9-3.5; after adjusting for age and immunocompromised status, OR = 3.5; 95% CI, 2.6-4.8). Specifically, cannabis users were more likely than nonusers to have one of the mold infections (OR = 3.4; 95% CI, 2.1-5.3; aOR = 4.6; 95% CI, 2.9-7.4) and other fungal infections (OR = 2.2, 95% CI, 1.4-3.3; aOR = 2.9; 95% CI, 1.9-4.5). Among those with fungal infections, cannabis users were younger than nonusers (median age, 41.5 vs. 56 years; P < .001); more likely than nonusers to be immunocompromised (43% vs. 21%; P < .001); hospitalized on the fungal infection diagnosis date (40% vs. 13%; P < .001) and have tobacco use codes on their insurance claim (40% vs. 9%; P < .001).

In addition, cannabis users who had fungal infections and unspecified cannabis use were more likely to be older than cannabis users who had dependence codes (median age, 52 vs. 28 years) and were more frequently immunocompromised (63% vs. 25%). Cannabis users who had fungal infections were less likely to have cannabis use or dependence codes than cannabis users who did not have fungal infections (60% vs. 79%) and unspecified cannabis use codes (48% vs. 29%).
The findings align with the American Society of Transplantation Infectious Diseases Community of Practice recommendation that solid organ transplant recipients avoid cannabis smoking, they added.
“Patients with other immunocompromising conditions should be also aware of the possible
link between cannabis smoking and fungal infections and might also consider avoiding this exposure,” Benedict and colleagues wrote. “Physicians should remain aware of the possible link between fungal infections and cannabis use.” – by Janel Miller
Disclosure: Healio Primary Care could not confirm relevant financial disclosures at the time of publication.